A 60 y/o female with SOB and cough
This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
The patient/ attender was informed the purpose of the information being acquired. An informed consent was taken from patient/ attender and there is omission of information that was requested to be omitted.
CHIEF COMPLAINTS
A 60 year old woman came to the OPD with chief complaints of
- shortness of breath since 10 days.
- Dry cough since 10 days.
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic 10 days ago, when she developed shortness of breath grade 2 mMRC, that was insidious in onset, gradually progressive, aggravated on exposure to cold and dust.
H/O of orthopnea, wheeze
No H/O paroxysmal nocturnal dyspnea
Dry cough is also present since 7 days, no aggravating or relieving factors present.
No H/O fever, chest pain, chest tightness, hemoptysis, sweating, palpitations
No H/O weight loss
PAST HISTORY
Similar complaints 10 years ago. Usage of rotahaler (Fluticasone + vilantrol)
Patient on Tab. Acebrophyllin 100mg PO/BD.
Patient on Diabetic medication.
No H/O TB, epilepsy, thyroid disorders, HTN, CAD in the past.
FAMILY HISTORY
Not significant
PERSONAL HISTORY
Diet - Mixed
Appetite - Normal
Sleep- Adequate
Bowel and bladder movements- Normal
Addictions - None
No known allergies seen.
TREATMENT HISTORY
Stopped diabetic medication since 5 days.
Inhaler usage since 10 years for asthma.
No H/O blood transfusions or surgeries.
GENERAL PHYSICAL EXAMINATION
Patient is conscious, coherent and cooperative.
With moderate built and nourishment.
Pallor - no
Icterus - no
Cyanosis - no
Clubbing - no
Koilonychia - no
Lymphadenopathy - no
Oedema - absent
VITALS
Temperature - Afebrile
Pulse rate - 100 bpm
Respiratory rate - 25 cpm
BP - 140/80 mmHg
SpO2 - 96% at room temperature
GRBS - 350 mg/dL
SYSTEMIC EXAMINATION
1) Respiratory System
Inspection :
Shape of chest - circular
Pectus excavatum seen
Position of trachea - central
Bilateral symmetrical chest expansion observed
Apical impulse
No visible pulsations/sinuses/scars seen
Palpation : (Confirming findings on inspection)
Trachea - central
Apex beat - normal
Respiratory movements - normal
Chest circumference - 22 inches
Vocal fremitus - normal
No tenderness over intercostal spaces
Percussion :
Resonant note heard bilaterally
Auscultation:
Vesicular breath sounds are heard.
2) CVS - S1, S2 heard ; no murmurs or thrills heard.
3) Abdomen - Scaphoid abdomen, no tenderness, no palpable mass, normal hernial orifices, no free fluid, no bruits
No palpable spleen or liver
4) CNS - All higher mental functions, cranial nerves, motor system and sensory system are intact.
Normal speech observed.
INVESTIGATIONS
Haemogram
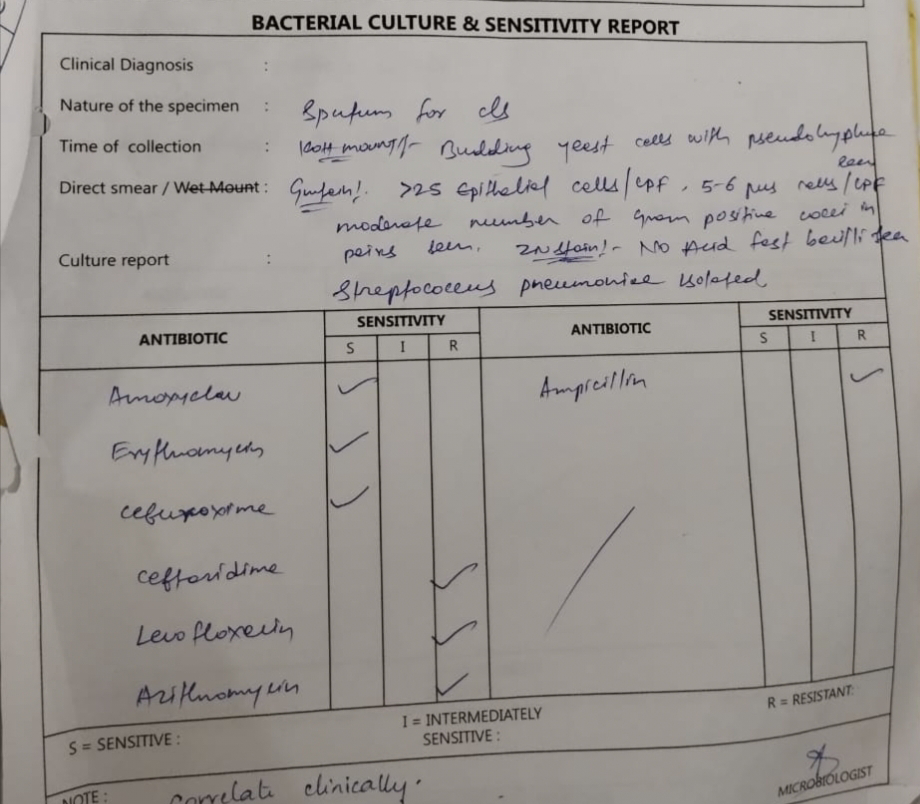
Bacterial culture & sensitivity report
2D ECHO
Urine analysis
PROVISIONAL DIAGNOSIS
Acute exacerbation of Bronchial asthma
TREATMENT
Inj. AUGMENTIN 100mg IV TID
Inj. PAN 40mg IV/OD
Inj. LASIX 40mg IV/BD
Inj. HEPARIN 5000 IU/IV/QLD
Inj. HYDROCORTISONE 100mg IV/BD
Inj. HUMAN ACTRAPID INSULIN S.C/TID
Inj. NPH S.C/BD








Comments
Post a Comment