48 year old male with Ascites and pedal oedema since 2 months
This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
The patient/ attender was informed the purpose of the information being acquired. An informed consent was taken from patient/ attender and there is omission of information that was requested to be omitted.
CHIEF COMPLAINTS
A 48 year old male came with chief complaints of
- Abdominal distention since 2 months
- Bilateral pedal edema since 2 months
-Decreased appetite since 2 months
- Decreased urine output since 1 month
HISTORY OF PRESENTING ILLNESS
Patient was apparently alright 2 months back then he developed abdominal distention which is insidious in onset gradually progressive associated with decreased appetite since then.
Bilateral pedal edema extending upto knee since 2 months , pitting type increased on walking and relieved with rest
Decreased urinary output since 1 month
No h/o fever, cough, breathlessness

PAST HISTORY :
No h/o DM HTN TB asthma epilepsy CVA CAD.
PERSONAL HISTORY :
Consumes 180ml alcohol occasionally and stopped 1 year back.
Smokes beedi 1 pack per day and stopped 3 months back
GENERAL PHYSICAL EXAMINATION:
Patient is conscious ,coherent and cooperative and well oriented to time, place and person.
moderately built and nourished.
Pallor-absent
Icterus -absent
Cyanosis-absent
Clubbing-absent
Generalised Lymphadenopathy-absent
Edema-bilateral pedal edema present
VITALS:
Temperature - 98.2F
PR :- 95bpm
RR : 22cpm
BP :- 110/70mm Hg
SPO2 :- 98%@RA
GRBS :- 110mg/dl.
SYSTEMIC EXAMINATION
Per abdomen -
Abdominal girth- 93-->91cm
Inspection-
Abdomen is distended , flanks are full, skin is stretched , no visible peristalsis , equal symmetrical movements in all quadrant’s with respiration
Palpation -
No local rise of temperature, no tenderness
All inspectory findings are confirmed by palpation, no rebound tenderness, gaurding and rigidity.
No tenderness , No organomegaly
Fluid thrill present
Percussion:
Shifting dullness present
Auscultation:
Bowel sounds heard
CVS : S1 and S2 heart sounds heard
CNS: NO focal neurological deficits
RR: BAE Present, normal vesicular breath sounds heard,no adventitious sounds
shape of the chest: normal
trachea appears to be central
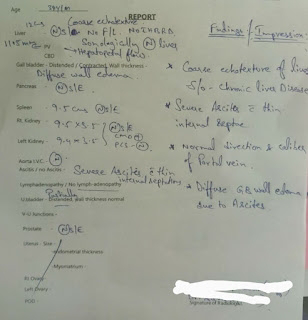
USG abdomen
PHES test
Interpretation
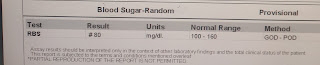
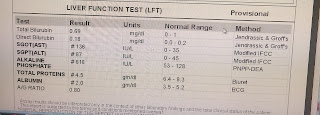
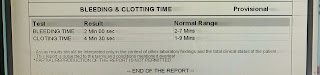
INVESTIGATIONS
Ascitic tap -
Appearance - clear , yellow coloured
SAAG - 1.65 g/dl
Serum albumin - 2.0 g/dl
Asctic albumin - 0.35 g/dl
Ascitic fluid sugar - 104mg/dl
Ascitic fluid protein - 0.7 g/dl
Ascitic fluid amylase - 17 IU /L
LDH : 143 IU/L
Cell count- 50 cells
Lymphocytes nil
Neutrophils 100%.
TREATMENT :
Tab LASIX 40 mg PO BD
Syp. Lactulose 10 ml PO HS
Strict Alcohol abstinence .



















Comments
Post a Comment